Pelvic Organ Prolapse
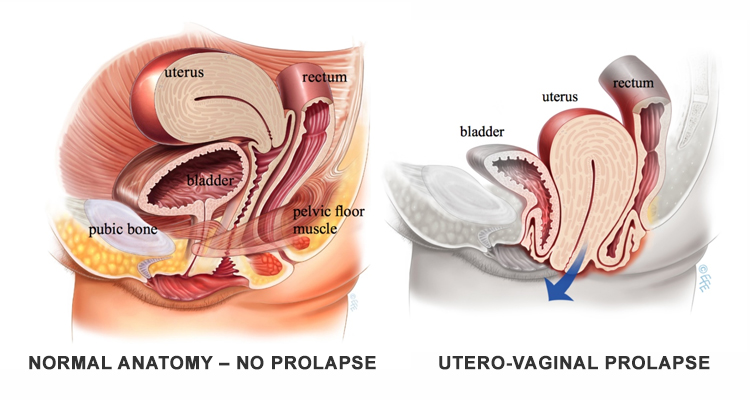
The organs within a woman’s pelvis (uterus, bladder and rectum) are normally held in place by ligaments and muscles known as the pelvic floor. If these support structures are weakened by overstretching, the pelvic organs can bulge (prolapse) from their natural position into the vagina. This includes the top of the vagina (vault prolapse) following a hysterectomy. When these organs descend, or herniate, it is known as pelvic organ prolapse. Sometimes a prolapse may be large enough to protrude outside the vagina.
Prolapse of the pelvic organs is common and affects the quality of life of millions of women. However, prolapse often does not require treatment, especially if there are no associated bothersome symptoms (see below).
Symptoms :
Prolapse may be noted incidentally during a vaginal examination by a healthcare professional e.g. during a routine cervical smear. If the prolapse is small or not causing any problems, no intervention is required.
Symptomatic pelvic organ prolapse refers to a change in sensation or function experienced by a woman in reference to the position of her pelvic organs. Symptoms are generally worse in situations when gravity might make the prolapse worse (e.g. after long periods of standing or exercise) and better when gravity is not a factor e.g. lying supine. Again symptoms may be more noticeable at times of abdominal straining e.g. defecation.
Women may experience one or more of the following:
- Vaginal bulging: Sensation of a ‘‘bulge’’, lump or ‘‘something coming down’’ or ‘‘falling out’’ through the vaginal introitus. The bulge may be felt by direct palpation or be seen, perhaps aided with a mirror.
- Pelvic pressure: A feeling of increased heaviness or dragging (pain or discomfort) in the suprapubic area and/or pelvis.
- Bleeding, discharge, infection: Abnormal vaginal bleeding, discharge or infection which may be related to ulceration of the prolapse. This is more likely to occur if the prolapse is protruding outside of the vagina.
- Splinting / Digitation: Some women may need to digitally push the prolapse back into the vagina or apply manual pressure to assist bladder emptying or defecation.
- Low backache: Complaint of an ache (‘‘menstrual-like’’) in the lower back associated with vaginal prolapse and relieved when the prolapse is reduced. Note: Low backache may have a number of different causes unrelated to prolapse.
Causes :
The main cause is damage to the nerves, ligaments and muscles which support the pelvic organs. Certain risk factors predispose to pelvic floor damage:
- Pregnancy and childbirth are considered to be major factors leading to weakening of the vagina and its supports. Prolapse affects about one in three women who have had one or more children. A prolapse may occur during or shortly after a pregnancy, or may take many years to develop. However, it is important to emphasise that only 1 out of 9 women (11%) will ever need surgery for prolapse in their lifetime.
- Aging and menopause may cause further weakening of the pelvic floor structures.
- Conditions that cause excessive pressure on the pelvic floor like obesity, chronic cough, chronic constipation, heavy lifting and straining.
- Some women may have an inherited risk for prolapse, while some diseases affect the strength of connective tissue e.g. Marfan syndrome and Ehlers-Danlos syndrome.
How Bad Is My Prolapse?
Many women (up to 40%) have a minor degree of prolapse with minimal or no symptoms. Your doctor will take a complete medical history and perform a vaginal examination to determine prolapse severity and grade.
What Treatment Is Right For Me?
There is no single best treatment for all patients. Treatment needs to be individualised and will depend on many factors including your history, symptoms, your doctor’s experience and your own personal preference.
Not all women need surgery. In fact, for some women, doing nothing may be a perfectly reasonable option. It may be that making simple lifestyle changes is all that is required or more conservative strategies such as supervised pelvic floor exercises may be beneficial. Other treatments such as vaginal pessaries to provide support or surgical repair of prolapse can be explored should the various conservative strategies be ineffective or unsuitable.